
Drexel Hill (484) 521-0233
West Chester (610) 436-5883

Drexel Hill (484) 521-0233
West Chester (610) 436-5883

 Rheumatoid arthritis is a disorder and form of arthritis in which the body’s immune system attacks the lining of the joints. This can cause pain and inflammation and over time can damage the joints and bone. Rheumatoid arthritis can occur in any joint in the body but often occurs in the hands, wrists, and feet. Symptoms include pain, stiffness, and inflammation. Other symptoms can include fatigue, numbness, fever, sweating, and weight loss. These symptoms can often come and go and can last for days or weeks. There is currently no cure for rheumatoid arthritis; however seeing a doctor, such as a podiatrist, if you are experiencing pain in your feet can help provide a diagnosis and treatment. Treatment options may include therapy, medication, and, in some cases, surgery.
Rheumatoid arthritis is a disorder and form of arthritis in which the body’s immune system attacks the lining of the joints. This can cause pain and inflammation and over time can damage the joints and bone. Rheumatoid arthritis can occur in any joint in the body but often occurs in the hands, wrists, and feet. Symptoms include pain, stiffness, and inflammation. Other symptoms can include fatigue, numbness, fever, sweating, and weight loss. These symptoms can often come and go and can last for days or weeks. There is currently no cure for rheumatoid arthritis; however seeing a doctor, such as a podiatrist, if you are experiencing pain in your feet can help provide a diagnosis and treatment. Treatment options may include therapy, medication, and, in some cases, surgery.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact the podiatrists of Dr. Siegerman & Associates. Our doctors will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Although rheumatoid arthritis attacks multiple bones and joints throughout the entire body, ninety percent of people who actually develop this condition usually do so in the foot or ankle area. Those who develop this kind of arthritis in the feet usually develop symptoms around the toes and forefeet first, before anywhere else. Rheumatoid arthritis appears to have a genetic component. If it runs in the family, then you will be more likely to develop it as well.
Rheumatoid arthritis is an autoimmune disorder in which the body’s own immune system attacks the lining of the membranes surrounding the joints. This causes inflammation of the membrane lining, and the gradual destruction of the joint’s cartilage and even bone.
Some of the most common symptoms that are associated with RA include pain and swelling of the feet. Stiffness in the feet is also another common symptom that people experience. Those who have RA in the feet usually feel the pain in the ball or sole of their feet. This can get to be very painful at times. A person's joints can even shift and become deformed after a period of time.
In order to properly diagnose RA in the feet it is usually necessary for a doctor or podiatrist to evaluate the area. Your doctor will also question you about your medical history, occupation, etc., to determine whether anything in your lifestyle may have triggered the condition. There are a number of tests that may be performed to help diagnose RA, such as a rheumatoid factor test. There is, however, no one single test that will tell you for sure if you have RA. There are different X-rays that can be taken as well to determine if a person has RA in their feet.
There is a range of treatment options for rheumatoid arthritis. Treatment of RA is usually a lifelong process that includes a variety of methods of treatment and therapy. Your doctor can prescribe special shoes that should help with arch support as well as heel support. A physical therapist can help those with this condition learn exercises which will keep their joints flexible. Surgery may be needed to correct some of the issues with the feet, such as bunions, and hammertoes. Fusion is usually the most successful surgical option for rheumatoid arthritis. However, people need to keep in mind that there are some risks associated with these surgeries.
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
 Athlete’s foot is a skin infection caused by fungus. As the name implies, it is common among athletes; this is mainly due to the fact that locker rooms, pools, and public showers are likely to harbor the fungus. The fungus also prefers moist, warm, and dark areas such as in between the toes on feet that are generally covered with shoes. While the infection usually first occurs between the toes, it can spread to the rest of the foot. Symptoms include redness, itchiness, burning sensations, and peeling skin. If scratched, the fungus can spread to other parts of the body like nails. To prevent athlete’s foot, keep your feet dry. If your feet sweat a lot, change socks frequently to prevent moisture buildup. Once you are finished showering or out of the pool, dry the feet thoroughly. Finally, wear shoes that allow the feet to "breathe” to help prevent sweat and allow the feet to cool down.
Athlete’s foot is a skin infection caused by fungus. As the name implies, it is common among athletes; this is mainly due to the fact that locker rooms, pools, and public showers are likely to harbor the fungus. The fungus also prefers moist, warm, and dark areas such as in between the toes on feet that are generally covered with shoes. While the infection usually first occurs between the toes, it can spread to the rest of the foot. Symptoms include redness, itchiness, burning sensations, and peeling skin. If scratched, the fungus can spread to other parts of the body like nails. To prevent athlete’s foot, keep your feet dry. If your feet sweat a lot, change socks frequently to prevent moisture buildup. Once you are finished showering or out of the pool, dry the feet thoroughly. Finally, wear shoes that allow the feet to "breathe” to help prevent sweat and allow the feet to cool down.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact the podiatrists from Dr. Siegerman & Associates. Our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
 Working out and building strength is a good way to help prevent running injuries. Here are a couple of workouts you can try to help build muscle in your feet and legs. Do each of these exercises for and 4 to 5 sets of 15 to 25 repetitions . Before you do these however, it is recommended you see a podiatrist first and ask if exercising is right for you. To do a toe-curl walk, stand barefoot and move forward with your right leg using only your toes, then do the same for the left foot; you will only move an inch or so while doing this. Heel raises are easy to do. Just stand up on your toes while keeping your heels off the ground for about 1 second and then come down. Chair squats are a good way to work your quadriceps. Place a non-rolling chair behind you, and squat down over it so that your butt only briefly touches the chair. Then come up. Finally, to workout your gluteus muscles, lay on your stomach and bend your knee at a 90 degree angle. Slowly raise your thigh off the ground for a couple of seconds, then bring down your thigh and repeat with the other leg. These exercises are quick and easy to do and will build strength that will further help prevent running injuries.
Working out and building strength is a good way to help prevent running injuries. Here are a couple of workouts you can try to help build muscle in your feet and legs. Do each of these exercises for and 4 to 5 sets of 15 to 25 repetitions . Before you do these however, it is recommended you see a podiatrist first and ask if exercising is right for you. To do a toe-curl walk, stand barefoot and move forward with your right leg using only your toes, then do the same for the left foot; you will only move an inch or so while doing this. Heel raises are easy to do. Just stand up on your toes while keeping your heels off the ground for about 1 second and then come down. Chair squats are a good way to work your quadriceps. Place a non-rolling chair behind you, and squat down over it so that your butt only briefly touches the chair. Then come up. Finally, to workout your gluteus muscles, lay on your stomach and bend your knee at a 90 degree angle. Slowly raise your thigh off the ground for a couple of seconds, then bring down your thigh and repeat with the other leg. These exercises are quick and easy to do and will build strength that will further help prevent running injuries.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries. If you have any concerns about your feet, contact the podiatrists of Dr. Siegerman & Associates. Our doctors will treat your foot and ankle needs.
How to Prevent Running Injuries
Many common running injuries are caused by overuse and overtraining. When the back of the kneecap starts wearing out and starts causing pain in your knee, this is commonly referred to as runner’s knee. Runner’s knee is a decrease in strength in your quadriceps and can occur if you’re not wearing properly fitted or supporting shoes. To prevent runner’s knee, focusing on hip strengthening is a good idea, as well as strengthening your quads to keep the kneecaps aligned.
What Are Some Causes of Running Injuries?
- One cause of a common running injury is called iliotibial band syndrome.
- Plantar fasciitis is also another common injury.
- Stress fractures can occur from overtraining, lack of calcium, or even your running style.
Best Ways to Prevent Running Injuries
- Wear footwear that fits properly and suits your running needs.
- Running shoes are the only protective gear that runners have to safeguard them from injury.
- Make a training schedule. Adding strengthening exercises as well as regular stretching can help keep you strong and limber and can lessen the possibility of injuries.
- Stretching keeps muscles limber; this will help you gain better flexibility.
If you have any questions please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
 Falls and their effects on the elderly are, unfortunately, not reported on enough. This lack of reporting prevents overall awareness and the spread of knowledge in how to prevent them. Fortunately this has been changing in the past several years, with 2008 marking the first year that Falls Prevention Awareness Day was held by the National Council on Aging (NCOA). Despite this, awareness of the issue has a long way to go. Here are some facts about falls and falls prevention. Those who are age 65 or older and who have been to the emergency department are unlikely to engage in falls-prevention programs once discharged. While it has been reported that regular strength and flexibility programs for the elderly help prevent falls, some practices like Tai Chi have been found to help as well. Finally, elderly persons who have a history of falls, have suffered from a previous fracture, and have a body mass index (BMI) of 20 kg/m² are more likely to suffer another fracture.
Falls and their effects on the elderly are, unfortunately, not reported on enough. This lack of reporting prevents overall awareness and the spread of knowledge in how to prevent them. Fortunately this has been changing in the past several years, with 2008 marking the first year that Falls Prevention Awareness Day was held by the National Council on Aging (NCOA). Despite this, awareness of the issue has a long way to go. Here are some facts about falls and falls prevention. Those who are age 65 or older and who have been to the emergency department are unlikely to engage in falls-prevention programs once discharged. While it has been reported that regular strength and flexibility programs for the elderly help prevent falls, some practices like Tai Chi have been found to help as well. Finally, elderly persons who have a history of falls, have suffered from a previous fracture, and have a body mass index (BMI) of 20 kg/m² are more likely to suffer another fracture.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with the podiatrists from Dr. Siegerman & Associates. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
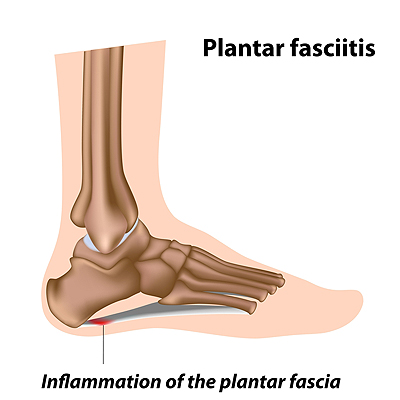 Many people who suffer from foot pain are diagnosed with plantar fasciitis, but what is it? Plantar fasciitis is the inflammation of the plantar fascia ligament in the heel. Symptoms consist of a stabbing or burning pain in the heel, which tends to worsen from overuse. Thankfully, it is a condition that can be treated. Typical causes of plantar fasciitis include repetitive movements from athletic activities, flat feet, obesity, age, and poor footwear. If you think you suffer from plantar fasciitis, see a podiatrist for a diagnosis. Treatment can include a simple change in footwear, orthotics, keeping pressure off the foot, and corticosteroids. Plantar fasciitis can be painful, but it is treatable with proper care.
Many people who suffer from foot pain are diagnosed with plantar fasciitis, but what is it? Plantar fasciitis is the inflammation of the plantar fascia ligament in the heel. Symptoms consist of a stabbing or burning pain in the heel, which tends to worsen from overuse. Thankfully, it is a condition that can be treated. Typical causes of plantar fasciitis include repetitive movements from athletic activities, flat feet, obesity, age, and poor footwear. If you think you suffer from plantar fasciitis, see a podiatrist for a diagnosis. Treatment can include a simple change in footwear, orthotics, keeping pressure off the foot, and corticosteroids. Plantar fasciitis can be painful, but it is treatable with proper care.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact the podiatrists from Dr. Siegerman & Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
How Can It Be Treated?
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
 Gout, a form of arthritis caused by uric acid crystals forming in joints, can be very painful and can occur in any joint in the body. Thankfully, gout can be managed with a good diet. Avoiding high intakes of acid-rich food is advised. Purines, which are converted into uric acid by the body, come from animal and plant foods. Purine-rich diets, especially from meat and seafood, increase the risk of gout attacks. While not completely preventing gout attacks, diets with plenty of vegetables do help. Low-fat dairy products have been found to prevent uric acid buildup as well. Alcohol has also been linked with dramatically increased rates of gout attacks, so cutting back on alcohol is a great way to prevent gout attacks. While improving your diet won’t eliminate gout, it will certainly help to lessen attacks and their effects.
Gout, a form of arthritis caused by uric acid crystals forming in joints, can be very painful and can occur in any joint in the body. Thankfully, gout can be managed with a good diet. Avoiding high intakes of acid-rich food is advised. Purines, which are converted into uric acid by the body, come from animal and plant foods. Purine-rich diets, especially from meat and seafood, increase the risk of gout attacks. While not completely preventing gout attacks, diets with plenty of vegetables do help. Low-fat dairy products have been found to prevent uric acid buildup as well. Alcohol has also been linked with dramatically increased rates of gout attacks, so cutting back on alcohol is a great way to prevent gout attacks. While improving your diet won’t eliminate gout, it will certainly help to lessen attacks and their effects.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact the podiatrists from Dr. Siegerman & Associates. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Request a free copy of
Laser Away Foot Pain!
today.
