
Drexel Hill (484) 380-9989
West Chester (610) 890-4609

Drexel Hill (484) 380-9989
West Chester (610) 890-4609

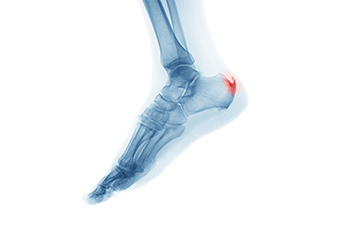
Heel spurs are bony protrusions that develop on the underside of the heel bone, often causing discomfort and pain. These spurs typically form in response to long-term strain on the ligaments and muscles of the foot, which leads to the calcification of soft tissues near the heel. While some individuals with heel spurs may not experience any symptoms, others may encounter persistent pain, especially during weight-bearing activities such as walking or standing. The pain is often described as a sharp, stabbing sensation in the heel. Inflammation and tenderness may accompany the discomfort, further affecting mobility. Seeking professional evaluation from a podiatrist is essential for an accurate diagnosis and the formulation of an effective treatment plan to alleviate symptoms and enhance overall foot health. If you have a heel spur, it is suggested that you consult with this type of doctor who can accurately diagnose and treat this condition.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact the podiatrists from Dr. Siegerman & Associates. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.

Cracked heels, a common and often painful foot ailment, may be more than a superficial concern. It could be a subtle indicator of underlying nutritional deficiencies. Essential vitamins like A, C, and E, along with minerals such as zinc, contribute significantly to skin health. Insufficient intake of these vital nutrients can compromise the skin's elasticity and integrity, leading to dryness and fissures, particularly on the heels. Vitamin A plays a vital role in skin regeneration, while vitamin C supports collagen synthesis, essential for maintaining skin suppleness. Vitamin E functions as an antioxidant, protecting skin cells from damage. Zinc aids in wound healing, essential for repairing cracks in the skin. Understanding the correlation between vitamin deficiencies and cracked heels highlights the importance of a well-balanced diet and, when necessary, nutritional supplements. If you have cracked heels, it is suggested that you confer with a podiatrist who address the problem and offer treatment options.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact the podiatrists from Dr. Siegerman & Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
Ways to Prevent Cracked Heels
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.

Red feet in the elderly can be a symptom with a myriad of potential causes. One primary contributor is reduced circulation, a common age-related issue that compromises blood flow to the extremities. Chronic venous insufficiency, where weakened veins struggle to return blood to the heart, may result in redness in the feet due to pooling blood. In some cases, medications or medical conditions affecting blood vessels can contribute to this discoloration. Additionally, inflammatory conditions like arthritis or infections might manifest as redness in the feet. Diabetic complications, particularly peripheral artery disease, may also lead to diminished blood supply and red discoloration. A podiatrist needs to conduct a thorough assessment to accurately diagnose and address the root causes of red feet in the elderly. If you or someone you know has this foot condition, it is suggested that you visit a podiatrist who can offer appropriate treatment options.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact the podiatrists from Dr. Siegerman & Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Many foot diseases and conditions become more serious and common among the elderly. Some of these conditions include diabetic ulcers, ingrown toenails, fungus, arthritis, corns, and calluses. Unfortunately, it may be harder for older adults to take care of their own feet, but there are some precautions they can take in order to avoid any serious conditions.
Dry, cracked heels tend to be a common problem for older people. In order to avoid this, you should always keep your feet clean and well moisturized. Special feet moisturizers should be used as average lotions might not provide enough moisture for dry and cracked heels. Daily foot inspections are crucial for the elderly to detect any irregularities in their earliest stages. During the aging process, blood circulation tends to slow down causing older people to not feel their feet as well as they used to. This often results in foot problems going unnoticed.
Fungal and bacterial conditions thrive on elderly feet because older adults are less likely to keep their feet clean and dry; this makes it easier for bacteria to take hold in their dry, cracked skin. Elderly people should be sure to thoroughly dry their feet, especially in between the toes, after bathing. This will help them avoid developing any fungal infections. Additionally, clean cotton socks should be worn after the feet are dried.
Cutting toenails straight across will help prevent ingrown toenails. When toenails are cut too lose, the nail might break through the skin resulting in an ingrown nail. Clippers should be used to cut the nails in order to make the cut even.
Elderly people who have diabetes are at risk of developing serious foot problems that may lead to amputation. Ulcers that are left untreated can lead to gangrene. Dry and cracked feet, fungus, and untended cuts under the nails may also lead to infections.
Fortunately, Medicare covers many different types of services for foot care. Elderly people with any of these foot conditions should seek the help of a podiatrist and perform daily foot inspections in order to ensure that they have healthy feet.

Diabetic wounds are a common complication of diabetes, resulting from neuropathy and vascular disease. Nerve damage diminishes foot sensation, making it challenging to detect an injury. Vascular disease impairs blood flow, which reduces the speed of healing wound. Diabetic foot ulcers are the most prevalent type of wound. They are open sores on pressure points, typically caused by neuropathy, trauma, and pressure. Early detection and treatment are essential to prevent infections and potential limb loss. Diabetic neuropathic wounds stem from nerve damage, leading to a loss of protective sensation. These wounds may appear as calluses, corns, or blisters, requiring specialized care to prevent infections and further damage. Ischemic wounds arise from an inadequate blood supply, often due to peripheral artery disease, or PAD, which is exacerbated by diabetes. Characterized by poor circulation and delayed healing, ischemic wounds pose an increased risk of infection. If you are experiencing frequent or stubborn foot wounds that will not heal properly or seem infected, it is suggested that you seek the help of a podiatrist for care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with the podiatrists from Dr. Siegerman & Associates. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.

Ingrown toenails in the elderly can result from various risk factors. These include both anatomical and behavioral factors. Improperly trimming or tearing nails, as well as wearing tight or ill-fitting footwear, can contribute to the development of ingrown toenails. The use of shoes, especially constricting ones, is associated with an increased risk. Systemic diseases, such as diabetes and obesity, may predispose individuals to lower extremity edema, making them more susceptible to ingrown toenails. Certain medications like retinoids, oral antifungals, and cyclosporine have also been linked to the condition. Hyperhidrosis, or excessive sweating of the feet, can soften the nail and skin, making it easier for the nail to pierce the surrounding skin. Poor foot hygiene can also exacerbate this issue. Repetitive trauma from activities like running or sports can be inciting factors for ingrown toenails. Some individuals may have a genetic predisposition or a family history of ingrown toenails. Additionally, congenital malalignment of the great toenails is associated with a higher risk of developing ingrown toenails. If you are a senior and suffer from discomfort of ingrown toenails, it is suggested that you schedule regular appointments with a podiatrist to obtain proper care and learn more about preventative measures.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact the podiatrists of Dr. Siegerman & Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact one of our offices located in Drexel Hill and West Chester, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown toenails (onychocryptosis) are a common foot ailment and it is very unpleasant to experience. The condition is caused by an increase in pressure from the ingrowth of the nail edge into the skin of the toe. Ingrown toenails commonly cause pain in those who experience them. In some cases, the skin surrounding the ingrown toenail may break which may lead bacteria to enter through and cause an infection. Common symptoms of this ailment include pain, redness, swelling, and warmth around the toe.
An imbalance between the size of the nail and the enlargement of the nail skin edge causes ingrown toenails. This condition is often caused by improperly trimming the toenails. If you are trying you cut your nails, you should always try to trim straight across instead of in a rounded shape. Ingrown toenails can also be an inherited condition and they may also be caused by improper shoe fitting.
Another common cause of the condition is wearing shoes that are either too small or too large. Other causes include poor foot hygiene, obesity, diabetes, arthritis, edema, and fungal infections. There are many risk factors that may make a person more likely to develop an ingrown toenail. Athletes who play “stop and start” sports such as tennis, soccer, and basketball are most likely to have ingrown toenails.
People who have diabetes, a compromised immune system, or poor circulation should immediately seek care from a podiatrist if they have an ingrown toenail. It is also recommended to seek professional assistance if at-home remedies are not successful within a week or if there is persistent pain.
Request a free copy of
Laser Away Foot Pain!
today.
